ELBOW PROCEDURES
ARTHROSCOPIC DEBRIDEMENT OF THE ELBOW
Overview
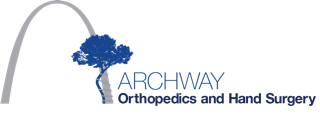
During this outpatient procedure, the surgeon examines the inside of the elbow joint with a camera called an arthroscope. The surgeon identifies and corrects problems with the bones, ligaments and tendons of the elbow.
Preparation
In preparation for the procedure, sedation or general anesthesia is administered. The elbow is numbed with a local injection.
The Examination
The surgeon injects fluid into the elbow to expand the joint and provide a clear view. The surgeon creates a series of small incisions in the skin around the elbow joint. The surgeon inserts an arthroscopic camera and other instruments into the elbow. The camera allows the surgeon to view the procedure on a monitor. The surgeon carefully examines the joint to look for signs of damage.
Repairing The Joint
Once the elbow has been diagnosed, the physician may use one or more of the arthroscopic instruments to repair the joint. Bone spurs may be filed down, and loose or damaged cartilage may be removed.
End Of Procedure
When the procedure is complete, the incisions are closed with sutures or surgical staples. The elbow is bandaged. The patient will be given pain relievers and should be able to leave the hospital the same day.
© Swarm Interactive, Inc.
ARTHROSCOPIC DEBRIDEMENT OF THE ELBOW
Aspiration of the Olecranon Bursa
Overview
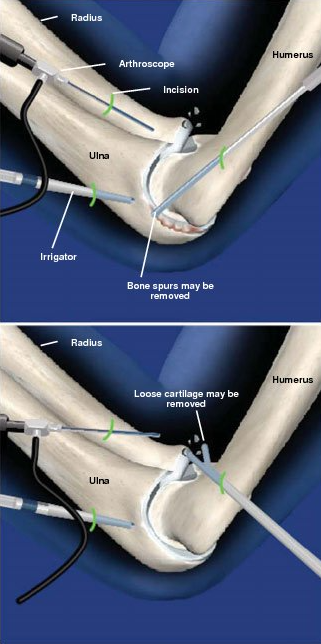
This outpatient procedure relieves pain and swelling in the elbow caused by bursitis, or inflammation of the bursa. The bursa is a fluid-filled sac between the skin and bones of the elbow.
Preparation
The patient is positioned so that the elbow can be bent comfortably, and the back of the elbow is cleaned and sterilized. Local anesthesia is administered to numb the injection site.
Removing Fluid
The physician inserts the needle and guides it into the affected bursa. The needle is carefully pushed into the bursa, and excess fluid is drained to reduce the swelling. Corticosteroid medication may also be injected in patients with chronic bursitis.
End Of Procedure
The needle is slowly withdrawn, and the injection site may be covered with a small bandage. Extended pain relief usually begins within two to three days of the injection.
© Swarm Interactive, Inc.
CUBITAL TUNNEL RELEASE AT THE ELBOW
Overview
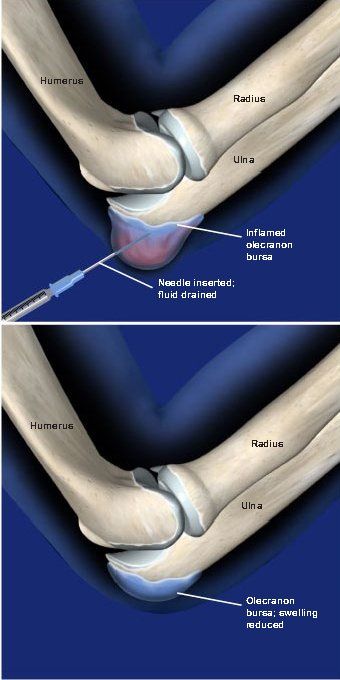
This outpatient procedure, performed under general or regional anesthesia, alleviates compression of the ulnar nerve. This nerve travels along the inner side of the elbow and down to the hand. Cubital tunnel release is used to treat cubital tunnel syndrome.
Preparation
Anesthesia is administered, and the patient is positioned to allow access to the inner side of the arm. The area is cleaned and sterilized.
Accessing The Joint
The surgeon makes an incision along the inner side of the elbow to access the cubital tunnel, the open space surrounded by muscle and bone that provides a channel for the ulnar nerve.
Relieving The Compression
The surgeon carefully opens the roof of the cubital tunnel at the site of the compression, creating more space for the ulnar nerve. The nerve is often moved out of the tunnel and repositioned along a new path to prevent it from being compressed in the future. If the nerve is compressed in multiple places, more than one section of the tunnel may require treatment.
End Of Procedure And Aftercare
The incision is closed with sutures, and the arm is bandaged and placed in a splint. The patient is allowed to go home the same day. Physical therapy may be required after the arm has healed.
© Swarm Interactive, Inc.
MEDIAL EPICONDYLECTOMY
Overview
This outpatient procedure, performed under general or regional anesthesia, removes the medial epicondyle (the bony bump on the inner side of the elbow) to alleviate compression of the ulnar nerve. Medial epicondylectomy is used to treat cubital tunnel syndrome.
Preparation
Anesthesia is administered, and the patient is positioned to allow access to the inner side of the arm. The area is cleaned and sterilized.
Accessing The Joint
The surgeon makes an incision along the inner side of the elbow to access the medial epicondyle. The ulnar nerve is carefully pushed clear of this bony bump.
Relieving The Compression
The surgeon cuts away the medial epicondyle to create more space for the ulnar nerve. This will allow the ulnar nerve to slide unobstructed along the bone when the elbow is bent.
End Of Procedure
The incision is closed with sutures, and the arm is bandaged and placed in a splint. The patient is typically allowed to go home either the same day or after an overnight stay.
Aftercare
The patient may be required to wear a splint for two to six weeks after the surgery. Occupational or physical therapy may be required after the arm has healed.
© Swarm Interactive, Inc.
ARTHROSCOPIC DEBRIDEMENT OF THE ELBOW
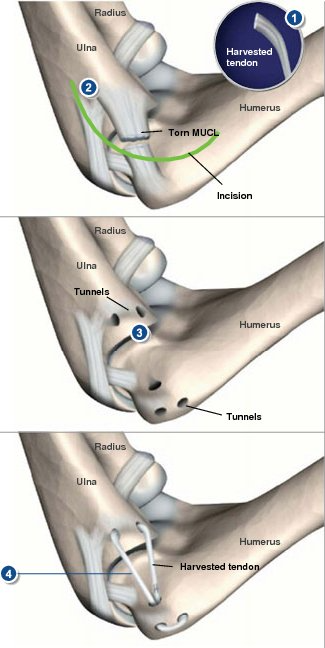
Medial Ulnar Collateral Ligament Reconstruction (Tommy John Surgery)
Overview
This procedure is designed to repair a torn elbow ligament - an injury typically caused by strong, repetitive overhead throwing motions of the arm or by dislocation of the elbow. It was first performed in 1974 on baseball pitcher Tommy John.
Preparation
The surgeon harvests a tendon from the patient's own body. The palmaris longus tendon of the forearm is most frequently used, but the surgeon may instead choose to take a tendon from the hand, wrist or knee. In some cases, a tendon from an organ donor may be used.
Accessing The Elbow Joint
The surgeon makes an incision along the inner side of the elbow, exposing the damaged medial ulnar collateral ligament.
Drilling The Holes
Tunnels are drilled through the humerus (upper arm bone) and ulna (a lower arm bone) at the points where the damaged ligament normally attaches.
Inserting The Tendon
The harvested tendon is looped through the tunnels in a figure-eight pattern. The tendon is sutured to itself, stabilizing the joint.
End Of Procedure
The incision is closed, and the elbow is immobilized in a hard brace for one to two weeks. The patient may then be allowed to switch to a hinged brace and begin limited exercise of the arm. Supervised throwing may begin at three to four months; competitive throwing may be allowed at six to nine months. Most athletes regain their pre-injury level of function about 12-18 months after surgery.
© Swarm Interactive, Inc.
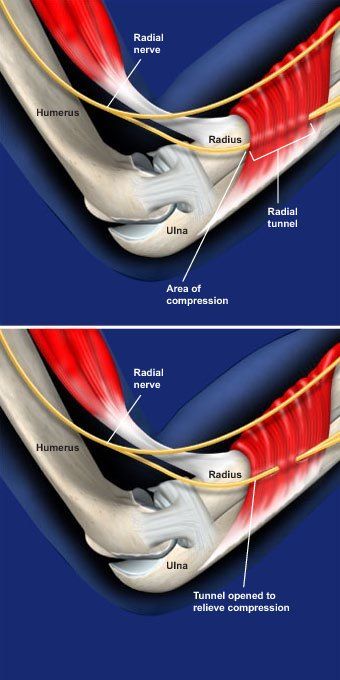
RADIAL TUNNEL RELEASE AT THE ELBOW
Overview
This outpatient procedure, performed under general or regional anesthesia, alleviates compression of the radial nerve. This nerve travels along the outer side of the elbow and down to the hand. Radial tunnel release is used to treat radial tunnel syndrome.
Preparation
Anesthesia is administered, and the patient is positioned to allow access to the outer side of the arm. The area is cleaned and sterilized.
Accessing The Joint
The surgeon makes an incision along the outer side of the elbow to access the radial tunnel, the open space surrounded by muscle and bone that provides a channel for the radial nerve.
Relieving The Compression
The surgeon carefully opens the roof of the radial tunnel at the site of the compression, creating more space for the radial nerve. If the nerve is compressed in multiple places, more than one section of the tunnel may need to be opened.
End Of Procedure
The incision is closed with sutures, and the arm is bandaged and placed in a splint. The patient is typically allowed to go home either the same day or after an overnight stay.
Aftercare
The patient may be required to wear a splint for two to six weeks after the surgery. Physical therapy may be required after the arm has healed.
© Swarm Interactive, Inc.
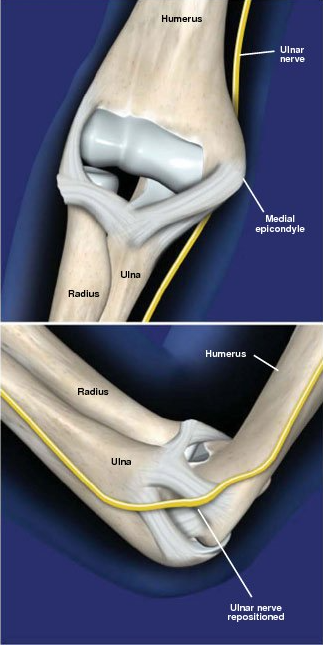
ULNAR NERVE TRANSPOSITION AT THE ELBOW
Overview
This outpatient procedure, performed under general or regional anesthesia, repositions the ulnar nerve to prevent it from sliding against or becoming pinched by the medial epicondyle (the bony bump on the inner side of the elbow). Ulnar nerve transposition is used to treat cubital tunnel syndrome.
Preparation
Anesthesia is administered, and the patient is positioned to allow access to the inner side of the arm. The area is cleaned and sterilized.
Accessing The Joint
The surgeon makes an incision along the inner side of the elbow to access the ulnar nerve and medial epicondyle.
Rerouting The Nerve
The surgeon carefully moves the ulnar nerve from behind the medial epicondyle to a new position in front of this bony bump. The nerve can be routed over, through, or under the muscles of the forearm. The new placement will prevent the nerve from being compressed against the medial epicondyle when the elbow is bent.
End Of Procedure And Aftercare
The incision is closed with sutures, and the arm is bandaged and placed in a splint. The patient is allowed to go home the same day. The patient may be required to wear a splint for one to two weeks after the surgery. Occupational or physical therapy may be required after the arm has healed.
© Swarm Interactive, Inc.